How Location Affects the Planning of Healthcare Facilities, Part 1
The planning of healthcare facilities must also consider and analyze how its location can affect the general design direction of the space. Here, we consider such factors as rural and urban sites, geography, and boundaries created for other reasons.
SPACE
Richard Lasam
7/29/20255 min read


A definite resource for me as an architect for healthcare facilities is this book by the World Health Organization:
WHO District Hospitals: Planning and Design – Chapter 2 Location
This is a resource that is free to be downloaded, and it is a great help to me in fixing certain portions of the design process for healthcare facilities, in this case—how to locate a healthcare facility. This is a long chapter in the book, so the elements of how location affects design are divided into three parts as listed here:
PART 1: Mapping Exercise and Service Catchment Area
PART 2: Factors to Be Considered in Locating a District Hospital (i.e. a Healthcare Facility)
PART 3: Site Selection
For this blog post, I will discuss PART 1, which is about doing mapping exercises and defining a service catchment area. Paragraphs in quotations are direct passages from the book—otherwise, the rest of it is how I utilize this book in my practice as a healthcare architect.
PART 1
1. Inventory and distribution of health facilities (mapping exercise)
As discussed in the book:
“One of the most effective ways of determining the location of a new facility is to use a base map of the district and vicinity, on which one can enter, translate and compare data, facts and information (Fig. 4). A basic mapping exercise is the first step in locating the positions of existing facilities; a graphical analysis of data on where patients come from can be used to determine the areas of influence and service of those facilities. This kind of analysis shows the overlapping of influence and any voids that need filling and therefore warrant the provision of a new facility.”
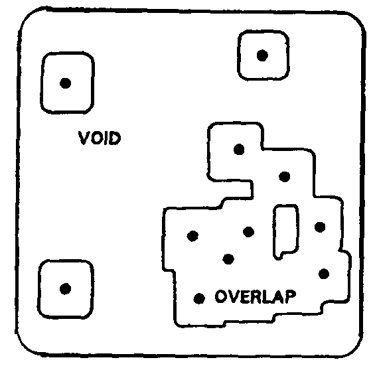
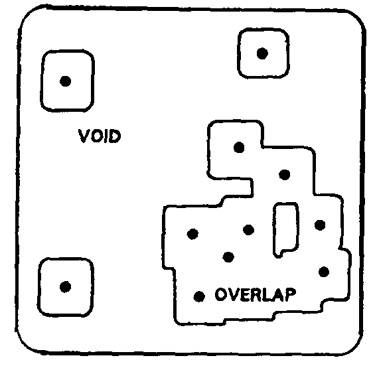
Figure 4. Mapping Exercise
What does this mean in terms of architecture? This is a site survey of the town, city, or region in which one will be building a healthcare facility. Depending on the facility being designed—be it a clinic, a diagnostic center, or a hospital—different parameters will be considered to determine the need for the healthcare facility in the specified area. How this specified area can be determined will be discussed in Part 2.
As an architect, I can ask these questions to determine the feasibility of the healthcare facility for the location: Are there too many similar projects around? Will there be enough patients to warrant the construction of this facility? How far away is the healthcare facility from other affiliated medical service providers that will aid in the operations of the project? Considering these questions helps the client to make an informed, objective decision as regards to how to adjust, expand, or whether it might be better to abandon the project. It is the duty of the architect to provide the client with enough information and analysis to say if it is viable to pursue a project—even if it results in the architect losing the project.
1. Service Catchment Area
The Service Catchment Area is the specific area in which a healthcare facility operates within physical space. The three boundaries that define these are:
a. “Political administrative boundaries are usually the strongest determinant, as they set a defined area and imply an established organization which directs, manages and operates the affairs of the population within its jurisdiction. In most countries, the hierarchy of physical facilities parallels that of the politico-administrative organization, so that a particular level of facility is under the jurisdiction of an equivalent level of the politico administrative unit throughout the country.”
The effect of this boundary is reflective on whether the healthcare facility is a government or private entity as well as if the healthcare facility is to be located in an urban area or provincial space. Some government healthcare facility may be dictated to serve only the citizens of its political unit. A privately owned healthcare facility does not necessarily limit who can use the facilities based on the political boundaries of the area. Again, this needs to be cleared up with the client before the design of the project can proceed.
If the area is urban, the urban space might be an isolated city so only that city is the service area of the healthcare facility. Or it might be located in a metropolis with multiple cities adjacent enough to each other to be within range of the service area.
In rural areas, perhaps the healthcare facility is the only one of its kind around a large portion of a region, hence it will service multiple political entities instead of only one.
b. “Geographical boundaries are natural physical barriers to population movement and can therefore also be strong determinants of catchment areas (Fig. 5). Mountain ranges and bodies of water, for instance, deter cross movement. People may cross politico administrative boundaries to reach a facility, however, if they are deterred by a natural barrier within their own district. Geographic boundaries are often formalized into politico administrative boundaries as a natural consequence of the development of ethnic, cohesive, or homogeneous cultures on either side.”
The effect of geographical boundaries is well explained in the book (as shown below)—so as an architect, one must be aware of the surrounding features that may affect the healthcare facility in terms of access by patients to the site of the project. One observation that I have seen in action is that certain types of road systems actually create a pseudo geographic boundary: usually, these are highways, bridges, and major roads. For example, the healthcare facility may be across the road, but if that road is a major thoroughfare and getting to the facility entails following the flow of the traffic to find the nearest U-turn just to turn back and get to the hospital, it is likely the patient will decide to go to a different place altogether.
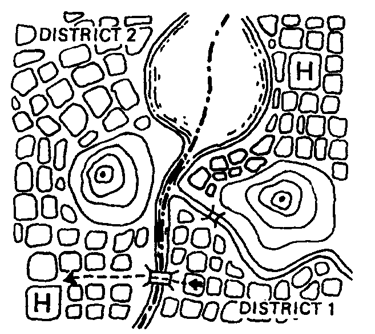
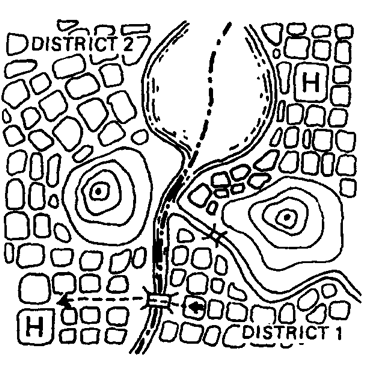
Fig. 5. Natural Physical barrier as a determinant of catchment area
a. “Time boundaries, although invisible, determine catchment areas in regions without roads and easy means of transport (Fig. 6). Populations gravitate towards the facilities that are most easily accessible, that is, the facility they can get to in the shortest time. The factor of geography also contributes to this situation, as difficult terrain takes longer to negotiate.”
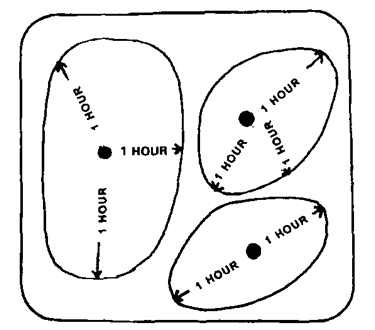
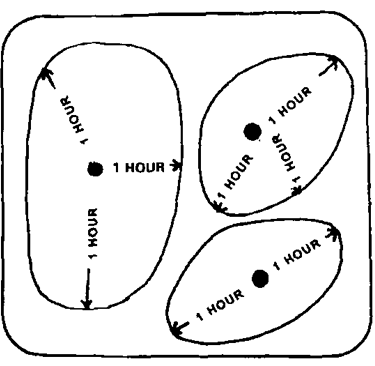
Fig. 6. Time boundaries as determinants of catchment area
This is an adjunct boundary to geographical boundaries as human nature will often make us travel to the nearest and easiest place to get a service. Time boundaries can be dictated by the various modes of travel, from walking, to bicycles, vehicular travel, and mass transit. A general rule is that if it takes longer than an hour to get somewhere, most people will consider spaces that can be accessed in a shorter amount of time. (Again, just because the hospital is closer “as the crow flies” doesn’t mean the patient will get there faster.)
Architects should advice clients if the healthcare facility project being designed may have challenges in terms of getting patients, visitors, and the medical staff to the location of the healthcare facility. Difficulties or impracticalities of getting to the healthcare facility will be detrimental to long term success and operations of the project if not addressed correctly.
I discussed another part of this book (specifically the Design Brief) in this blog post (https://www.spaceandcare.com/nine-elements-your-design-brief-must-have ) if you want to read more about this specific publication.
Parts 2 and 3 will be a future blog post.
